Comparisons in genital mucosal immune cell populations, gene expression, and impaired anti-viral immunity in women with and without female genital schistosomiasis before and after praziquantel treatment




Other Research Programmes

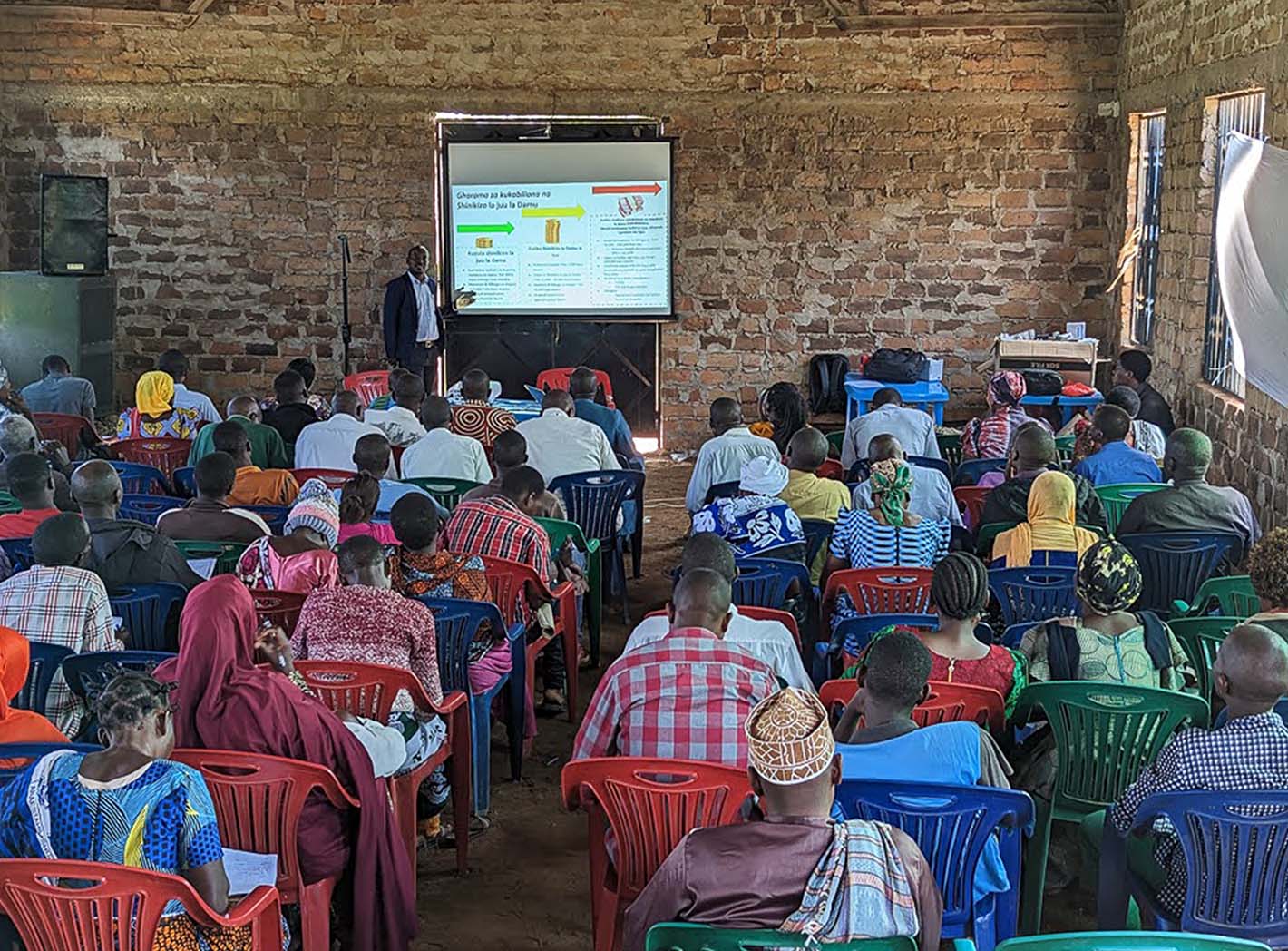
Daraja Trial
Reducing Post-Hospital Mortality in HIV-infected Adults in Tanzania (Daraja Trial)

Vijana Check study
Reaching adolescents with health services: a multi-country study of adolescent health check-ups in low and middle-income countries (Y-Check study)

Mwanza HIV&HTN Sleep Cohort
HIV, Sleep, Nocturnal Non-Dipping, and Cardiovascular Disease: A Tanzanian Cohort (Mwanza HIV&HTN Sleep Cohort)
Reduce BP in Tanzanian communities
Engaging Religious Leaders to Reduce Blood Pressures in Tanzanian communities

DoRIS trial
A dose reduction immunobridging and safety study of two HPV vaccines in Tanzanian girls (DoRIS trial)

Add-Vac study
Adding a Male Single Dose HPV Vaccination to Female HPV Vaccination in Tanzania (Add-Vac study)

Female Genital Schistosomiasis
Comparisons in genital mucosal immune cell populations, gene expression, and impaired anti-viral immunity in women with and without female genital schistosomiasis before and after praziquantel treatment

PASS-MHW
Partnering to support schools to promote menstrual health and wellbeing among secondary school girls in Tanzania (PASS-MHW) project